Insights on Breast Cancer Treatment: Yuan Yuan, MD’s Discussion on Sacituzumab Govitecan and Other Novel Treatments
Today we’re gonna take this chance to review breast cancer immunotherapy and novel drug antibody conjugates. This is my disclosure, so. So let’s, when we talk about breast cancer immunotherapy, we’re gonna start with triple negative breast cancer,no-brainer because triple negative breast cancer is currently the only space we have. FDA-approved immunotherapy now talks about a triple negative breast cancer.
You all know that it’s a very challenging disease despite all the improvement we made so far. We’re still far from curing every single subtype. So if you look at triple negative breast cancer, why it’s so difficult is because there has been lots of tor heterogeneity from multiple levels. For example, if you look at the early.
mRNA
mRNA classifier from the left side of the screen. You can see that from the early pembrolizumab 50 to Layman’s. And then moving on to bursting with these classifiers, they don’t agree with each other. So these are based on the mRNA profiling. So you can divide them into basal, like, basal, like one and two methylation, linal androgen receptor subtype, but then in the middle panel really showcase from primary breast cancer diagnosis.
You follow the same patient through time in a time of metastatic disease diagnosis. You can see it. A majority of the tremors do not stay the same. There has been a phenotype shift and to add the complexity of the story DNA Clonality also changes. New clones arise, old clones disappear. And then last, not the least, the DNA methylation also made it the expression level furthermore.
Metastatic Triple-negative Breast Cancer in Comparison
Okay, so going to the metastatic triple-negative breast cancer in comparison with lionel versus other subtype, you can see that the patients with metastatic triple-negative breast cancer does have slightly, you know, maybe perhaps the molecular features make them prompt to respond to immunotherapy higher pills, higher PD-L1 expression.
And perhaps increased tor mutation burden. So based on the triple negative breast cancer or microenvironment, you can further break them down into fully inflamed, stoma restricted margin, restrict and immune desert. So, That surely sort of set a foundation for understanding of the responses to neoadjuvant therapy.
So this is a Keynote 522 trial, neoadjuvant therapy incorporating immune checkpoint inhibitor pembrolizumab in early stage, high risk, triple negative breast cancer therapy. And noted that in this trial basically by adding. Immune checkpoint inhibitor pembrolizumab versus the placeboto the chemotherapy backbone with carboplatin taxol followed by ac.
And then if you look at the fireleft panel, you can see the pathological complete response rate,which is the holy grail of neoadjuvant therapy in triple negative breast cancer, has a significant increase at delta of about 14%by adding immunotherapy. And interestingly , the PDL one does not dominate the more objective response rate.
If you look at the middle panel here is at the PD-l1. Regardless of PD-L1 status, positive or negative,, you can still see a consistent. Responses from immune checkpoint inhibitors, but that has not yet translated to overall survival benefit due to limited observation time and follow up time.
But three years , invasive disease-free survival has significantly improved and far. Right. You see the forest plot basically showed across different subtypes or features. Patients unanimously benefit from the treatment. Now beyond the pembrolizumab, you know that there’s a few other immune checkpoint inhibitors currently undergoing rigorous clinical trials testing.
This includes atezolizumab and also dramatic mad. You see that the delta PCR significantly improves with the incorporation of an immune checkpoint inhibitor. But with that being said, the recent trend of treating early stage high-risk advanced breast cancer, we observed cross different subtypes. We’re basically escalating the therapy for Trone negative in the post neoadjuvant setting.
We’re adding more chemo for HER2 positive. We now have extended HER2 targeted therapy. HR positive, HER2 negative disease we have extended , beyond five years. Now some patients get 10 years of therapy, including addition of CDK4/6 inhibitors. So that’s a challenge about escalating therapy.
But do we need to do that for every single patient? So what if the patient does not fit for eny? So this is a great trial recently presented at the ASCO, looking at a non-answer cycling regimen using a single agent, single arm. carboplatin docetaxel plus pembrolizumab and the far left in the box, you can see that with the addition of pembrolizumab , to the.
, double. It’s here only every three weeks for six cycles. Patient gets a pretty decent PCR of 58%. So, although the limitation of the studies is relatively small the total number of patients is small, and follow up is relatively short. So this is what I kind of came up with a recentCN guideline and incorporating what we had at cters.
, so the purple box you can sort of neglect. These are the clinical trials. We’re planning to activate a cters, but this is sort of an algorithm to treat early stage, high risk , triple nine breast cancer. You’ve noted that we didn’t have time to go over everything, but on the right hand side. Sowe know that earlier we have the adjuvant capecitabine data.
Can we continue capecitabine for those patients?
Can we continue capecitabine for those patients? Didn’t achieve pcr and just simply added pembrolizumab. How aboutBRCA one and two populations when they have. Residual disease. We have single agent data of Olaparib, but we actually do not have adjuvant olaparib plus pembrolizumab in a combination trial. But I think we’re extrapolating from the best data possible.
And this is a sort of you know, based on the early phase 1/2 combination clinical trials in this drug , combination that showed safety. So, Using it. But bear in mind they do not have a large , phase three randomized clinical trials when combining pembrolizumab in the adjuvant setting with these agents. And then inwe, we will talk a little bit about ISPY 2 trial, which is a really novel way to incorporating.
Novel therapies in the very early setting
Novel therapies in the very early setting. Instead of waiting for the usual development pipelines, you are moving from metastatic disease to the early stage to adjuvant and then into the early stage,we will discuss the Sando five in the next few slides. So this is what we have currently at Cedars not at advertising for us, but based onDr. Has Kar and Steven. Shiao trial, they incorporated a few years ago using single agent pembrolizumab. immunotherapy radiation therapy and the early line setting before the patient launched in standard care chemotherapy in their small size trial. The PRO trial actually demonstrated pretty promising PCR rate of 74% and building on this experienceI know we have friends from insights here, so there is a new trial, just got activated combination therapy with radiation plus pembrolizumab and css, one receptor inhibitor in the neoadjuvant setting.
So ISPY 2.2 reallydo not have time to go over that. It’s a really very intelligent way to incorporate your novel agents. If you see that from the bottom in the past two decades, I BY two has graduated multiple agents and the fast readout and does not take hundreds of patients, thousand patients to get signal.
Then you can quickly, swiftly move on to, to your best reasonable design. So Isy now, Moving on to the ISPY 2.2 version. I know UCSD groups are very actively involved in ISPY 2.2. So now it’s basically based on the baseline mammaprint results and then strategizes patients to multiple experimental therapy.
And then there’s interim pausing to assess rebiopsy based on the MRI finding. calculate the predicted PCR rate. So if the predicted PCR is there, the patient can go straight to surgery instead, you know, if the patient does not predict to have a good PCR, then they move on to the next section, blocked B and block C treatment.
So this is a really nice, innovative way to hopefully one day we can really tailor our therapy instead of just laying out. carboplatin taxol AC plus pembrolizumab, and then which does come with toxicity. So I think this is a future direction , personalized treatment for our neoadjuvant early stage patient.
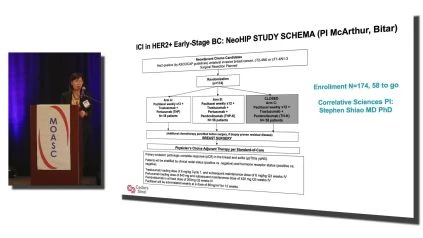
And , beyond the triple negative, we do have a current ongoing study testing the pembrolizumab in addition to neoadjuvant Paclitaxel, trastuzumab Pertuzabin. Er, po. Sorry for the HER2 positive , early stage breast cancer patient. The ongoing study here,now moving on to a metastatic setting. We know that Keynote 355 has led to the FDA accelerated approval of pembrolizumab in the frontline , specifically PD-L1 positive defined by the combined.
Positive score CPS score over 10% in that population with a modest progression-free survival benefit, but yet translated to overall clinical benefit. So in the box you can see the PFS benefit was 9.7 versus 5.6 months,so how, how does that impact our clinical care? Now in reality, approximately 30 to 40% of the metastatic triple negative breast cancer patients were PD-L1 positive.
You know, that not everybody would fit. And also because of the shifting landscape, we actually do not have data. In, you know, in the, in the, toward the fast. I would say in the next two, three years when our patient relapses after neoadjuvant chemo plus pembrolizumab, when they become metastatic, what are the patient’sor characteristics?
Are they still gonna be PD-L1 positive? That’s a really largely unanswered question. So I think, what’s this? , Trial is informing us that a lot more work needs to be done in order to, you know, perhaps induce more immune hot tor to be able to leverage an immune checkpoint inhibitor in a broader population in our triple negative breast cancer.
, so this is one of the strategies. You’re familiar with PARP inhibitors. Currently we have two PARP inhibitors specifically for BRC oh one and two mutated tours which are crossed in different groups, but within triple negative, about 10% of the patients were b C one positive. And it’s interesting that in the preclinical setting, I apologize for a really small font here.
Try to pack everything into one slide. You can see that PARP inhibitor actually is an immune activator. It can activate the sting pathway. Interferon gamma. So it’s potentially synergistic with immune checkpoint inhibitors. A number of clinical trials that’s been run, including olaparib plus Durvalab and also Niraparib plus pembrolizumab to PAI trial, which included patients who may not necessarily carry journal BRC M mutation.
They can be just you know, regular triple negative, perhaps have the. So these clinical trials sort of informed us that yes, there’s potential synergy,hopefully more study will be verified in this finding. And , this is my colleague Monica’s study at Cedars activating right now is Olaparib plus Pembrolizumab.
, but the instance specifically in h Rd, positive population. So I think we’re still currently enrolling. and this is an i i t coming finally getting activated after a long eight months of wait,it will be activated next week. SoIvermectin, I’m sure show off your hand probably, you know, through the pandemic or bad media for Ivermectin.
But , ivermectin actually is a drug being treated. Since the 1970s it has been used, over 700 million people around the world to treat, you know, specific parasites, river blindness. So through the work of my colleague at City of Hope, Dr. Peter Lee Lab, they’re doing a very rigorous NCI. Drug screening program identified that yes, ivermectin actually is an immune activating agent.
From the laptop left, you can see the immune cold tor. Not much of the tor infiltrating lymphocytes. After ivermectin exposure, you can convert these immune cold tor to immune hot. The change of tor microenvironment perhaps will promote potential responses to immune checkpoint inhibitors, and it’s clearly demonstrating the mice study.
Here. And then you can see that, you know, in the, in the , far right B panel, when tor disappeared in the mice, when you try to re-challenge with tor cell implant, more tumor cells, these tor actually do not grow. So this is very interesting. So because of this exciting finding, we were able to secure funding from Gateway Foundation.
We designed this , phase 1/2. Trial combining Arain with basil, which is an anti PD one inhibitor,we’re taking adult patients, who potentially already, you know, are no longer responding to immune checkpoint inhibitors. They can have a previous immune checkpoint. Inhibitor exposure and it was metastatic disease and we’re collecting biomarkers, blood, and microbiomes, and hopefully we’ll be able to enroll.
And , moving on to novel antibody drug conjugates. So you have heard a lot and I think the audience will ask questions. What is the T-DXd efficacy in non small cell lung and advanced breast cancer without HER2 mutations? So here we’re gonna limit our discussion into breast cancer. We have lots of excitement. So after the initial antibody drug conjugates, which is TDM one, now we have a plethora of agents and there’s more agents on the pipeline.
So we now have Sait o vCAN. We haveT-DXd We are gonna touch upon a little bit of petru, which is a, her three ADC was direct tamp payload. And then with recent FDA approval, we have expanded. Now, you know, to a new category, HER2 low and for home receptor positive, HER2 negative disease. We finally have a quite crowded ADC.
So I think what’s next is a sequential question that we will have to figure out how to address now. This is a very first phase three ascent trial. Prior to ascent, there is an earlier study. Phase 2 already demonstrated progression-free survival benefit and led to Sacituzumab Govitecan cancer accelerated approval.
So again, this is a phase three confirmatory study, confirming the progression-free survival benefit, and also you can see the data translated to overall survival benefit. This is now NCCN category one in metastatic breast cancer setting, triple negative breast cancer, and , This is the TROPiCS-02 presented last year at Asthma and San Antonio breast meeting looking at a heavily pre-treated hormone receptor positive, HER2 negative recurrent inoperable metastatic breast cancer.
Sacituzumab Govitecan versus dealer’s choice
So noted these patients, 100% of them progress through CDK4/6 inhibitors. And , beyond that they are. Received chemotherapy and the lines of chemo were 2 24 lines of treatment. Prior to enrollment to this trial, chemotherapy group of about 500 patients were randomized one to one to receive Sacituzumab Govitecan versus dealer’s choice, which includes a RET single agent, gemcitabine, orbin.
So look at the patient population. They’re against heavily pretreated lines of therapy. In the red box is zero to eight. From Sacituzumab Govitecan group and for GPCs, one to five and medi, three lines of treatment. And they have a heavy, you know, disease burden. 95% of the patient has visceral metastasis. Liver meat was really high.
, percentage, 84 to 87. and , knowing that, you know, the TROPiCS-02 did show a very modest, but yet significant , the median duration of progression-free survival 5.5 in the Sacituzumab Govitecan versus TPC 4.0 months, and the landmark progression-free survival rate is more pronounced. If you look at 12 months, 21% of the patients on Sacituzumab Govitecan did not progress, in contrast with 7% in the TPC arm.
And interestingly, this modest PFS clinical benefit. Did translate to a more pronounced median overall survival, benefit of differences of three months. So again, this is interesting data. Now it’s adding our moment to the whole receptor positive, HER2 negative disease,currently there’s ongoing clinical trials to, to really test a number of questions.
One is, what about moving this agent to upfront for frontline PD-L1 negative and positive population? So, ascent oh three and oh four is gonna address that question and more. So recently we were approached by the ASCENT05 trial, which is looking at patients who had undergone neoadjuvant standard care treatment.
Infor early stage triple neck breast cancer, but did not hit pcr. So in the adjuvant setting for those high risk patients, can we do better than single agent chemo? So the randomizations between sacituzumab plus pembrolizumab versus Standard care capecitabine plus pembrolizumab. So hopefully we will have a readout soon.
Sacituzumab Govitecan to be used as a frontline chemotherapy
And Ascend oh seven is moving beyond the ascent sorry, the TROPiCS-02 trial, so TROPiCS-02. We are looking at a heavily pretreated population, but Ascend oh seven. Were literally looking at Sacituzumab Govitecan to be used as a frontline chemotherapy when a patient had progressed after all , endocrine treatment.
When they move on to. So this is gonna push over the Zalo a bit to the side, but again, that’s a comparison norm. So this is a trial that will be initiated. So, I don’t believe anyone talked about Dato-TXd today. So Dato-TXd is a Trop two directed antibody drug conjugate with a payload of Diux tecan.
So somewhat the payload is the same as the T-DXd, but also belongs to the Topoisomerase inhibitor here, the drug antibody ratio. Different,1 28 for T-DXd. Here is 1 24. The linker is somewhat similar. So Data Dxt had undergone VI testing and trion breast 01 trial,you can see that in this cohort ofTriple negative cohort.
You see only 44 patients, but a heavily pretreated population. You see the waterfall plot has an excellent overall response rate of 34%. And uniquely, you know, think about this. TD X Dwe would think about i l D risk, but in this trial there’s no i l D and , it’s a unique difference moa. Perhaps the patient does have oral mucositis.
So Troon breast oh two and oh three is ongoing, and Troon breast oh three is sort of competing with Sacituzumab Govitecan to be used as a frontline chemotherapy in that post neoadjuvant residual cancer burden positive patient. And currentlyis also, you know, on the verge of activation. So there’s a number of other ongoing clinical trials of ADCs. So I want you to know, bore you, but.
I think we’ll keep our eyes open for future ad. . So HER2 low, we know that HER2 low disease has really changed how we used to categorize breast cancer into three buckets. But now we’re kind of, we’ve gotta be very careful and medical and clinical oncology, oncologists write their notes. HER2 negative is truly negative.
We do need to go back to dig our pathology findings. To really get the fine details or HER2 zero plus a zero one plus two plus or amplification. So I like to call HER2, pause the patient. Now HER2 amplifies it. So this is a huge impact. Look at the pie chart. Orange is too low. It counts for over 50%.
Cross different reports can be up to 55 to 60% of all commerce, there has been, you know, on the site we didn’t have time to present the data, but there has been interesting research looking. Is she a unique biology entity? So far we actually do not have that, that evidence,so I see my time is running out.
T-DXd
I’m gonna hurry up a little bit. So the T-DXd phase one B trial in her low breast cancer showed great efficacy and , overall response rate is 44%. And that led. Destiny Breast for four clinical trials, looking at T-DXd versusphysicians of Treatment choices in initial design was just to look at receptor positive, HER2 negative patients, but they were, you know, the, I have to recommend the sponsor.
It was really someone recommended to amend the study to add only metastatic triple negative breast only, so only 60 patients with triple negative breast cancer were included. But the results are remarkably different. So you can see that. And because the data is so well known, I wanted to take much more time. You already know that it’s a largely positive trial, progression-free survival and overall survival is significantly improved in that heavily pre.
Pretreated population looking at a triple negative, again, remarkable n equals to 58. You can see the progression-free and OS clinical benefit rate again in this very heavily pretreated population. So because of the data so strongAugust, 2022 F FDA approved T-DXd in HER2 low disease regardless of estrogen receptor status.
Okay, so D trial is really probably more provocative than we thought. So how low is low? So in the DAISY trial included patients with HER2 zero and they found that there is about 30% of response rate. So this is a really unaddressed question. There’s probably in the future we’ll hear about HER2 low, her ultra low patients.
, but at this moment, please don’t treat your HER2 zero patient withT-DXd. So , moving on to the next one is Petru Map. It’s her three targeting antibody drug conjugates again in a heavily pretreated population. In this trial, it was a dose finding. Study showed a significant benefit. Looking at t tmbc in the red box, you see a significant improvement and their income pneumonitis rate here.
, so stay tuned for this agent. So we don’t have time for this. So metastatic triple negative breast cancer treatment algorithm kind of updated based on the current NCCN guideline,we are a little bit closer to personalizing the treatment based on what patients have. ,so the, I know I, the topic was to look at, I’m running out 35 seconds.
Sothere’s a recent FDA approval for the novel estrogen receptor down regulator. Arin, I thought is, we should include that. So Amerid trials a phase three randomized trial, looking at aran versus investigator’s choice,Aromatase inhibitor, tamoxifen Fulvestrant. The data was fairly interesting.
You can see that patients are heavily pretreated. About a third of the patients previously received the injectable form of estrogen receptor down regulator Fulvestrant. And , 100% of the patients received CDK 46 inhibitors. But look at the patient’s key outcome here in e esr one mutated population progression-free survival.
Were 3.8 versus 1.9 months and had a ratio 0.55. And there’s an interesting landmark,if you look at the recent data analysis updated in the San Antonio breast cancer meeting, and it depends on how the patient performed on the previous CDK4/6 inhibitor. If there. you know, less aggressive tor biology or CDK 46 inhibitor exposure over 18 months.
ESR1 mutated population
You can see a really pronounced difference here in the population, the ESR1 mutated population. So again, 8.6 versus 2.0 months. So that led to FDA approval of the SS trend in ES r y mutated population. Currently, a multi-arm study called Elevate is ongoing. Combined LSS trend with either CDK4/6 inhibitor or P three C A inhibitors and also otherold everolimus in this multi-arm clinical trial.
Try to understand efficacy in the all comers of ER positive disease, not necessarily limited to S R Y mutation. So here’s this current landscape of home receptor positive, HER2 negative medicine, breast cancer treatment frontline, no-brainer. We’re talking about CDK4/6 inhibitors, and I know there’s a recent NCCN guideline update to move.
Ribociclib two category one for aromatase inhibitor combination. Andwe know that there’s overall survival differences between the three cdk,and then in the second line setting depending on the findings of p x three ca or ESR 1 mutation, we finally have some guidance there. And on the far right, do not forget that there has been.
Pembrolizumab and T Track fusion
Some tor agnostic indications here, including the MSI high DMMR patient with pembrolizumab and T Track fusion. I do find them in the genomic testing results, although extremely rare. And then we are really busy. A crowd beyond second line chemotherapy groups. That ADC is coming in expecting more ADC to come into the space, and then the sequeNCIng becomes a real challenge for the future.
And I was recently informed that there’sI think MD Anderson’s conducting a study. sequeNCIngdifferently. So T-DXd followed by Sacituzab Govitecan or Sacituzab Govitecan, followed by T-DXd. Hopefully we will have these results to guide our own clinical trials in practice. So I think I won’t repeat the conclusion here, but we are definitely making progress although far, far, far from enough compared with our.
Diffuse large B-cell lymphoma Dr. Budde presented and also Dr. Salgia presented a fascinating landscape of non small cell lung cancer lung cancers.
About the Author Yuan Yuan, MD, MPH – Cedars-Sinai Hospital:
CEDARS-SINAI APPOINTMENTS
-
Director, Breast Medical Oncology
Cedars-Sinai, Medicine
-
Medical Director, Breast Oncology Disease Research Group
Cedars-Sinai, Medicine
-
Director, Breast Medical Oncology
Cedars-Sinai, Cancer Institute
-
Medical Director, Breast Oncology Disease Research Group
Cedars-Sinai, Cancer Institute
DEGREES
-
PhD
University of California, Riverside, Riverside, United States
-
Medical Degree
Xuzhou Medical College, Xuzhou, China
CERTIFICATIONS
-
Medical Oncology
American Board of Internal Medicine, Philadelphia, United States