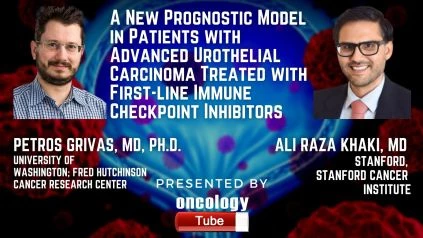
Petros Grivas, MD, Ph.D. Department Of Medicine, Division Of Medical Oncology, University of Washington; Fred Hutchinson Cancer Research Center, and Ali Raza Khaki, MD Stanford (Clinical Assistant Professor, Medicine – Oncology) speaks about A New Prognostic Model in Patients with Advanced Urothelial Carcinoma Treated with First-line Immune Checkpoint Inhibitors.
Link to Article:
https://www.sciencedirect.com/science/article/abs/pii/S2588931120302145?dgcid=author
Summary
Background information –
Although immune checkpoint inhibitors (ICIs) are approved in the first-line (1L) setting for cisplatin-intolerant patients with PD-L1-positive tumors or for platinum (cisplatin/carboplatin)-intolerant patients, reaction rates are modest and results are variable, with no clinically useful biomarkers (except for PD-L1).
The goal is to –
In a multicenter cohort study, we aimed to create a prognostic model for overall survival (OS) in patients receiving 1L ICIs for advanced urothelial cancer (aUC).
Participants, environment, and design –
This research involved patients treated with 1L ICIs for aUC outside of clinical trials from 24 hospitals in five countries (the United States and Europe).
Measurement of outcomes and comparative analysis –
To create a new risk score for patients receiving ICIs in the 1L setting, we used a stepwise, hypothesis-driven approach with clinician-selected covariates. Demographics, clinicopathologic data, treatment habits, and overall survival (OS) were all gathered in a consistent manner. Based on published data, a Univariate Cox regression was performed on 18 covariates that were hypothesized to be associated with OS. If variables associated with OS (p 0.2), were held for multivariate analysis (MVA) and used in the final model if MVA yielded a p 0.05. To construct a probability ranking, points were allocated to retained covariates depending on the beta coefficient. The C-statistic and stratified median OS is determined.
Conclusions and drawbacks –
The study involved 357 patients with an average age of 71 years, 27 percent of whom were female, 68 percent of whom had pure UC, and 13 percent of whom had upper tract UC. On MVA, success status 2, albumin 3.5 g/dl, neutrophil: lymphocyte ratio >5, and liver metastases were all important prognostic variables that were factored into the risk ranking. The latest 1L risk ranking had a C index of 0.68 (with a 95% confidence interval of 0.65–0.71). The retrospective nature of the study and the lack of external evidence are all drawbacks.
Final thoughts –
Based on evidence from patients with aUC treated with ICIs outside of clinical trials in the United States and Europe, we established a new 1L ICI risk score for OS. The components of the score emphasize easily accessible considerations specific to tumor biology and patient response. The aim is to get external recognition.
Description of the patient –