Ovarian Cancer Treatment: What to Watch for In New and Novel Trials Shannon Westin MD
By Shannon Westin, MD, MPH from MD Anderson Cancer Center
I’m so excited to be here. I love these virtual meetings, but I miss seeing all of you in person. I hope to be, uh, actually at the actual meeting next time. But without further ado, I’m really excited to review quite a bit of data with you today. I think that we’ve got lots of information and lots of exciting things. It’s really going to dovetail nicely with Dr. Cabelli’s talk.
So, without delaying any further, these are my disclosures: I work in drug development, so I work with all the companies. But just like my kids, I do not have a favorite. Other disclosure, there’s no way I can cover everything cool that’s going on right now in ovarian cancer, and I’m gonna try. So, it’s gonna be a lot of information but I’ll, uh, try to hit the high points for you. But I just want you to leave with a sense of hope and that sense that we always love to have here at Overcome, that there is more coming down the pike every single day. And so we hold on to that hope and know that we’re going to continue to find a cure for this disease.
So, with that, you’ve already gotten a recurrent ovarian cancer really nice primer on ovarian cancer. But I just wanted to give you a thought. I’m going to focus on recurrent ovarian cancer, not because I think that’s the most important place. I think every single part along the treatment continuum is important, but because a lot of our drug development happens in recurrent ovarian cancer and then we move it up front. Things like PARP inhibitors started in recurrence and then moved up front, and so there’s a lot of excitement about what we see in the recurrence setting and how it might be impactful even earlier and hopefully cure more patients.
As a reminder, the amount of time that it takes after upfront platinum to when there’s a recurrence gives us a sense of what might work, and where we really do a lot of our drug development is in that so-called platinum-resistant group, where our chemotherapy it’s only been about three to six months since the completion of chemotherapy before the cancer comes back. Response rates sit at about 20%, and let’s just refresh response rate means shrinkage of disease. And so we’re always looking to improve that bar, to improve the amount of time which it takes for cancer to grow, and that’s that PFS or progression-free survival.
Exploring Four Overarching Topics in Ovarian Cancer Treatment
So, I’m going to go through probably about four different overarching topics that have been explored to some degree in ovarian cancer. Again, it’s not all of the potential options, but some of the things that I’m most excited about. So first, anti-angiogenic agents. These are agents that target the vasculature, the blood supply to the tumor, and they cut it off while also targeting the cancer directly. Bevacizumab is the best-known and arguably the most well-established drug in this space. Many of you might have received it either in the upfront setting in combination with your chemotherapy or in the recurrence setting when Platinum is not an option, specifically in the Platinum resistance setting. We look at the Aurelia trial, which took standard chemo and added bevacizumab to it, and found that people lived longer without their cancer coming back, showing improved progression-free survival. You can see that curve on the left. For those of you who have seen me talk before, I’ll remind you that if you can get your thumb in between the curves, that’s a positive result. So this was a positive result, and importantly, patients felt better, and patient-reported outcomes were better when we added bevacizumab. However, as you can see from these curves, more and more patients progress as time goes on, and that is a problem. So we do want to explore how to overcome resistance to bevacizumab, one of our best agents. One of the things that we’ve explored is drugs that act on known mechanisms of resistance. Specifically, there’s a pathway called Notch that has been found to be active in tumors that are bevacizumab resistant. So we tried to block it with something called DLL4. When we blocked it by itself, it was pretty good. When we blocked it with bevacizumab, it was okay. But when we did a combination of the two, bevacizumab and DLL4, wow, it was really cool. Furthermore, if we added chemo, it was even better. So we took that into a clinical trial, and on the left, there was a drug called Nav6, a dual DLL4 and VEGF inhibitor. When we looked at it as a single agent, it had a 25% response rate, which is similar to chemo, so that’s not too shabby. But when we combined it with paclitaxel, standard chemotherapy, the response rates approached 33% for people who had received Avastin and 64% for people who had not, indicating a very nice active drug. This drug is moving forward in a phase three trial that will be open soon, comparing it to weekly paclitaxel.
What about Antibody-drug Conjugates in Ovarian Cancer Treatment?
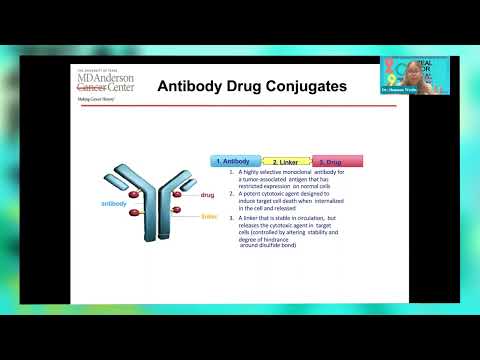
Now let’s talk about antibody-drug conjugates. This is an area that I’ve been very passionate about, and for those of you who have seen me speak before, you’ll remember this. Antibody-drug conjugates are one of the next frontiers for personalized medicine, really teasing out what is going on in your tumor and using a drug to target it. So, as a reminder and for education purposes, there are three pieces to antibody-drug conjugates. The antibody piece is the one that finds your cancer, acting as a key that goes into the lock of your cancer. Once that lock and key mechanism happens, it brings the drug inside, and that drug is a high-dose chemotherapy, something I could never give you in your vein or by mouth. But it brings that high-dose chemotherapy into the cancer and boom, it explodes and kills the cancer and also the abmornal cells around it. Very cool, right?
Why is this Important in Ovarian Cancer Treatment?
And what’s really cool about this is that you can have different antibodies, so you can have different keys to fit different cancer locks. I’m not going to go through this table in detail, but just know that there are many antibody drug conjugates and targets that are exciting in ovarian cancer. I’m going to talk to you about some of the drugs that are furthest along. The first is mervitaximab, which I’ll call Merv. This drug has been explored in ovarian cancer for a while. Early phase one clinical trails showed a really nice reduction, just like we saw with the last drug. However, the first randomized trial that compared mervitaximab to any chemo didn’t show a positive result, and we were all completely shocked. It turns out it was because we didn’t use the target or check the lock well enough. So those two curves on the top, oops, were basically showing us that you can’t fit your thumb in there. But when they did a better job of testing for the lock, the folate receptor Alpha, which is what this drug targets, then you can see some nice separation. This drug went on to be studied further in two different trials: the Soraya trial and mirosol. Mirasol has not yet been reported, but Soraya has, and Soraya led to an FDA approval for our patients. So, if your tumor has that lock, the folate receptor Alpha, you can receive mervitaximab, and you can see that the benefit was about a 30% reduction in tumor. But more importantly, look at these little swimmer plots. Each lane represents a patient, and how long she stays on the drug is her lane. You can see patients stayed on for over a year and a half to two years.
When this drug works, it can work very well. Importantly, it has shown effectiveness in people who had PARP inhibitors and in those who had multiple lines of therapy. This led to FDA approval. If you haven’t had your tumor tested for this, you need to talk to your doctor. I’m happy to talk to them on your behalf and arrange the testing.
Upifitamab Rilsodotin in Ovarian Cancer Treament
Now, let’s discuss another exciting drug called Upri, or Upifitamab Rilsodotin. However, for simplicity, let’s refer to it as ‘Upgrade.’ It’s an antibody drug conjugate that targets a calcium phosphate transporter known as Nappy To Be. It also contains a high-dose chemotherapy payload called AFHPA. The drug’s efficacy is being evaluated through tumor testing in an early phase trial, with a particular focus on ovarian cancer. The researchers identified the Nappy To Be lock as an important target for ovarian cancer, and they observed a significant reduction in tumors. In the waterfall plot shown here (a graph demonstrating tumor reduction), most patients experienced benefits, including tumor reduction or disease stabilization. Interestingly, the middle dose group demonstrated the best results, indicating that a higher dose didn’t necessarily correlate with better outcomes. Consequently, the dose of 36 milligrams per kilogram has been chosen to proceed with ongoing trials in patients with platinum-resistant ovarian cancer who have undergone one to four lines of therapy. This trial is actively enrolling participants, with the goal of obtaining FDA approval. Let’s keep our fingers crossed for another antibody drug conjugate!
Immunotherapy in Ovarian Cancer Treament
Okay, now for something completely different: immunotherapy. Immunotherapy utilizes the immune system to treat cancer and fight diseases. So far, single-agent immunotherapies haven’t been very effective against ovarian cancer, especially high-grade tumors. However, there have been some benefits observed in rare tumor types like clear cell. Thus, we are still searching for the right approach to immunotherapy for ovarian cancer.
Nemvaleukin alfa in Ovarian Cancer Treament
Enter Nemvaleukin alfa, a remarkable drug. It is an engineered cytokine that helps stimulate the immune system. Typically, cytokines are difficult to administer intravenously due to their side effects, such as fevers and chills, which can make patients feel unwell. However, Nemvaleukin alfa stands out because it minimizes systemic side effects. It offers the benefits of immune system stimulation without the unpleasant adverse effects.
In a study called Artistry One, nimbalukin was administered alone and in combination with pembrolizumab, an immune checkpoint inhibitor that stimulates the immune system. This combination proved to be well-tolerated, with reasonable safety profiles. Although some adverse events occurred, serious ones were observed in less than 50% of patients, and most were expected for cytokine-based chemotherapy. The study, albeit small, showed significant reduction of disease in many patients. Additionally, the treatment demonstrated long-term effectiveness.
Currently, the Artistry 7 study is underway, exploring the combination of Nemvaleukin alfa with pembrolizumab in a phase three study. This combination may be the breakthrough for immunotherapy in ovarian cancer. However, if it doesn’t prove successful, there is another exciting technology called adoptive cell therapy. In this approach, the patient’s own fighting T cells (immune cells) are extracted, modified to enhance their effectiveness, and then reintroduced into the bloodstream to observe positive outcomes. This technique is known as CAR T cell therapy. Several CAR T cell therapies are being investigated, but the one showing the most promise for ovarian cancer patients is a straightforward one called tile ADP A2 M4 cd8.
So, this is a CAR T Cell Therapy that focuses on a specific target called Mage A4, similar to the concept of lock and key with antibody-drug conjugates. In the early phase study called SURPASS, they observed a significant reduction in overall disease for patients whose tumors expressed this target. This therapy has the potential to activate the body’s immune cells to fight cancer in a more targeted manner. Notably, patients with ovarian cancer, particularly those with Mage A4, experienced a reduction in disease or clinical benefit, as shown in the top-left section of the waterfall plots. This promising development is now moving into a phase three trial, which indicates its proximity to FDA approval. It’s worth noting that most of the drugs discussed so far are also progressing to phase three trials, adding to the excitement.
PARP Inhibitors in Ovarian Cancer Treament
Moving on to PARP inhibitors, there are a few more points to cover, and I’m mindful of the time as we approach lunch. Please bear with me for another five minutes while I discuss some of my favorites. We mentioned earlier the goal of combining PARP inhibitors with other agents to overcome resistance and expand the number of patients who can benefit. Various mechanisms have been explored, such as activating alternative pathways to sensitize tumors to PARP inhibition, including PI3 kinase and ATR inhibitors. While time constraints prevent me from delving into the scientific details, it’s important to highlight that these options are entering phase three trials, which is incredibly exciting as it may enable more patients to benefit from PARP inhibitors in a successful manner. Lastly, I’d like to touch on a few other targets of interest that I find particularly exciting. One such target is Relicorlin, which takes a completely different approach by leveraging physiology against ovarian cancer. Cortisol, a natural steroid in our system, suppresses immune oxidation and aids tumor growth. By blocking the natural cortisol with a glucocorticoid receptor inhibitor like Relicorlin, we potentially help patients like you fight ovarian cancer. The study reported by Dr. Larusso demonstrated the effectiveness of Relicorlin in combination with chemotherapy, using an intermittent dosing schedule. These findings provide hope and open new possibilities for improving patient outcomes.
And when combined with chemo, it was found to be more effective than chemo alone. The Relic correlates in a continuous way, so again, looking at that, you can get your thumb in between the green and blue. That was a positive trial, so there’s a phase three trial enrolling right now. Another potential option quickly: AVB 500 is an axl inhibitor, which basically binds to a ligand called gas six. This is highly expressed in ovarian cancer and has been shown to contribute to metastasis and tumor genesis, leading to bad outcomes for patients with ovarian cancer. So we want to block that bad guy, and when we combine it with chemo, it’s safe, and the response rates approach 40%, which is extremely exciting. So there is a phase three trial with that drug. Now for Something Completely Different: this stuff is really cool. So this little machine, you place these pads on you, it’s called tumor treating Fields. It exerts these electrical fields that change our tubulin protein, and that is exactly what chemo does, actually, that’s exactly what toxins like paclitaxel will do. So you’re getting a chemo-like effect just by utilizing this machine with electric fields, and it disrupts the formation of your Montage spindle. It’s been very exciting; it’s actually FDA approved in glioblastoma as well as mesothelioma. So we thought, why not try to hit the tumor where it hurts in two places? So disrupt the mitotic spindle with paclitaxel and with tumor treating fields, and in a single-arm study, it seemed to work very well. Guess what? Phase three trial. This trial is done enrolling, and we’re eagerly anticipating the report on this. But hopefully soon, we’ll all be wearing little backpacks, treating our cancers while we walk around shopping. So the bottom line, the future’s bright, we’ve got a lot to talk about. I didn’t even get into everything I wanted to, just being mindful of our time. So we’ll have to get together again so I can go through everything else. But we have a lot of opportunities for patients with ovarian cancer. If you are actively receiving treatment, I encourage you to consider clinical trials and to talk to your practitioner about what options might work for you. And of course, I’m happy to talk to all of you at any time and answer any questions. Thank you so much for your attention.
10 Key Takeaways On the Discussion on Ovarian Cancer Treatment
-
Ovarian cancer treatment is an evolving field: Ongoing clinical trials are investigating new and innovative approaches to improve outcomes for ovarian cancer patients.
-
Combination therapies: Researchers are exploring the potential benefits of combining different treatment modalities, such as chemotherapy and targeted therapies, to enhance the effectiveness of ovarian cancer treatment.
-
PARP inhibitors show promise: Poly ADP-ribose polymerase (PARP) inhibitors have demonstrated significant efficacy in treating ovarian cancer patients with BRCA mutations and are being evaluated in various clinical trials.
-
Immunotherapy in ovarian cancer: Immunotherapeutic agents, such as immune checkpoint inhibitors, are being studied to harness the body’s immune system to fight ovarian cancer cells, leading to improved responses and durable remissions.
-
Maintenance therapy: Maintenance therapy with PARP inhibitors, particularly for patients who have responded well to initial treatment, has shown potential to delay disease progression and improve survival rates.
-
Targeted therapies: Targeted therapies that specifically inhibit key molecular pathways involved in ovarian cancer growth and progression are being investigated, with the aim of delivering more personalized and effective treatments.
-
Biomarkers for treatment selection: Identifying reliable biomarkers can help tailor treatment decisions for ovarian cancer patients, enabling more precise therapies based on individual characteristics.
-
Genetic testing: Comprehensive genetic testing is crucial in ovarian cancer management to identify inherited genetic mutations that may impact treatment decisions and inform risk assessment for patients and their families.
-
Novel treatment strategies: Researchers are exploring novel treatment strategies, including combination therapies with immunotherapies, targeted agents, and chemotherapy, to overcome treatment resistance and improve patient outcomes.
-
Clinical trial participation: Participation in clinical trials is vital for advancing ovarian cancer research and offering patients access to potentially breakthrough treatments that may not be available through standard care.
Shannon Westin, MD, MPH – About The Author, Credentials, and Affiliations
Shannon Neville Westin, M.D., is a medical oncologist, and a renowned clinical investigator specializing in developmental therapeutics and the utilization of biomarkers to forecast response and recurrence in gynecologic malignancies. She holds the esteemed positions of co-leader of the Ovarian Cancer Moon Shot™ and director of Early Drug Development in the Gynecologic Oncology department. Dr. Westin fulfills the pivotal role of principal investigator for numerous groundbreaking national and international clinical trials aimed at pioneering innovative treatments for gynecologic cancers.