Lung Cancer Trials: Insights into Latest Clinical Trials in Thoracic Oncology – Expert Analysis from Ravi Salgia, MD
By Ravi Salgia, MD, PhD
Thank you. After that introduction, I think my time is over, we can take questions now. If I can have my first slide. So for today, it’s a whirlwind of a talk to talk about lung cancer and we’ve certainly come a long way, but I’ll try to emphasize EGFR, KRAS, ALK and immunotherapy for non-small cell lung cancer. Lung cancer, as is a quite devastating illness. I’ve been in practice for over 33 years now and been practicing thoracic oncology and we know that it can metastasize to any organ. These are some of these representative examples and it is the leading cause of death. And unfortunately, about 2.2 million new cases will be diagnosed and 1.2, 1.8 million deaths worldwide, which is just quite devastating. And we need to make a difference in the context of lung cancer. And it’s not just about smoking. We live in California, not too many smokers or a lot former smokers potentially. But we are seeing non-smoking population with lung cancer, and that’s really important for us to realize not only is it a worldwide issue, it’s a United States issue, as well as, you can appreciate, it’s the number one cause of death among cancers for men and women. So it is also a woman’s disease as well.
Over my career, we know that lung cancer has come a long way in terms of its classification. Initially it was just one disease. Then we had mis subtypes, histologically, be it non-small cell lung cancer and small cell lung cancer. Then adenocarcinoma, squamous cell carcinoma, large cell carcinoma, and small cell carcinoma. But then precision medicine really has defined further what lung cancer is and should be and how we should potentially treat. So we know that there’s a lot of heterogeneity. I really don’t consider lung cancer as lung cancer anymore. It’s a cancer that arises within the lung with molecular abnormalities, with non-genetic abnormalities, with proteomics abnormality, and we have to be able to realize that this is a compilation of the data set from City of Hope, where we were able to look. The gender, race, smoking age ethnicity, as well as the various mutations that can occur. And in this tile plot, you can truly appreciate that we see a lot of EGFR patients here in Southern California, but we also see a lot of other patients with other molecular abnormalities such as KRAS or ALK. And these are some of the things that we’ll talk about in a few minutes. I think if you can really understand this slide, this lecture is over. And truly what we wanna be able to say is there are so many different therapeutic strategies we utilize lung cancer, molecular evolution is incredibly important, the tumor heterogeneity is incredibly important, and these slides certainly are all available to you and I’m happy to share them as well. But you can appreciate in the non-squamous cell condition. Predominantly for adenocarcinoma, you can have EGFR mutation, but you can go down that pathway and to be able to say, are there EGFR mutations in Exon19, or Exon21 or Exon20? And there are also N-terminus Exxon deletions that can occur or abnormalities that can occur that we’re identifying ALK fusions. There are over 15 ALK fusions known, and how do we challenge ourselves to the therapeutic decision making? ROS1, METex14, quite important in the context of how we decide therapeutics NTRK, BRAF, RET, and then we also have to look at the PD-L1 expression. How important is that in the context of non-therapeutic targets and then coming up with the immuno-oncology and immune-therapeutics themselves. And we’ll talk about a few of these as well.
So let’s talk about EGFR first. EGFR is a receptor tyrosine kinase located on chromosome seven. It’s very important as a tyrosine kinase, as the engine of the cell, and it interacts with many other receptors itself, such as the ErbB family, but it also interacts with MET and other receptor tyrosine kinase. But the systems’ biology, as you can see in the circle, is you can have a Ras/Raf pathway, B activated, PI3K activated, STAT pathway activated, but ultimately genetic alterations that can occur that leads to increased proliferation, decrease apoptosis, increase invasion, increase metastasis, and that’s why EGFR therapeutics was quite important for us, as we discovered in the context of non-small cell lung cancer. First generations were Gefitinib and Erlotinib. Many of you have experience with that. Then it was Afatinib and Dacomitinib. And thereafter, Osimertinib, Lazertinib has not been approved here in the United States, but certainly in South Korea. And now we have these fourth generations, such as the blue drugs themselves.
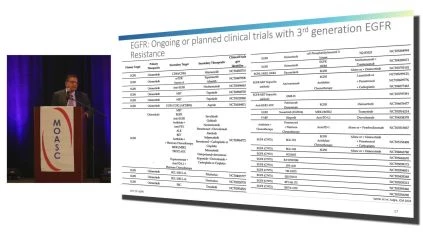
Here’s a timeline of FDA approvals. I won’t read this whole slide, but to be able to say EGFR was identified as a receptor kinase in the 1970s. And at the same time, the tyrosine kinase domain mutations were identified, which led to therapeutic targeting, and we’re quite excited that we have all of these options available, such as Erlotinib, Gefitinib, Afatinib, as well as Osimertinib and others that are coming to fruition. So what are some of these options for some of our patients? We know that osimertinib is a first line option for common EGFR mutations, and the most common EGFR mutations one has to consider is L858R, and Exon21, as well as Exon19 deletions. And you can see this in the survival curve, as you can see on the ordinance, is the overall survival on the emphasize, months to randomization and the curves do separate with a hazard ratio of 0.8. It’s also important to realize in a lot of artificial intelligence is going into that, that p53 alteration can inhibit sometimes the Osimertinib responses as well. p53 alteration with RB alteration can lead to small cell or neuroendocrine phenotype after certain months of Osimertinib. So you have to be considerate and cognizant of that for your patients, and then even in Exon19, not all Exon19s are created equal. You can have the 746 versus the 747, you can have the L-P abnormalities in Exon19. And all of those, we really take into account in our clinical decision making, sometimes we not only give Osimertinib as a first line, but we tend to combine it with chemotherapy as well, depending on the p53 and which domain of p53 is abnormal. Again, more and more new data is emerging that we have to be cognizant of that. We also know that Osimertinib has been approved for adjuvant non-small cell lung cancer. You can see the curve separating on the left. In terms of the d f s on the ordinance on the left, as well as with stage IB to 3A on the right end, panel B, it’s quite significant and we utilize that in our clinical practice as well. But we talked about L858R as Exon21. We talked about Exon19, but there are different Exons that can be abnormal. Most recently, the code is being broken for Exon20. So Exon20, not all Exon20s are created equal, but certainly. Agents such as Mobocertinib, as you can see here, has been FDA approved, as well as, Amivantamab that has been FDA approved as well. However, there are issues in terms of they don’t have as much of response in terms of duration of response as compared to agents such as osimertinib. And we have to be cognizant of that. We also know that we might have to combine it with chemotherapy in first line setting, and those lung cancer trials are actually ongoing. But I think the most important message, if I can send out today, is there are genetic and non-genetic alterations as mechanisms of resistance. We have to be aware of, we’ve all been taught, or we’ve all been ingrained to be able to say that there are genetic alterations. So as an example, With Osimertinib, you can have a C797S abnormality, you can have RAF fusions. You can also have MET amplification about a third of the time with Osimertinib. But those are all genetic changes. But what we didn’t appreciate except starting from the past few years, we’re starting to appreciate their non-genetic mechanisms of alterations. So MET expression itself, so protein expression can be abnormal. There are, you can see in this cartoon diagram, oncogenic EGFR mutation, genetic I just talked about, but the non-genetic, you can have cell phenotype changes. So going from non-small cell lung cancer, yeah, to small cell lung cancer or sarcomatoid or spindle cell cancer or squamous cell carcinoma, and those are important. You can have MET expression IGFR expression. You can also have this phenotypic switching. That’s really important in the plasticity, so keep that in mind as we go forward. I think some of you might have seen CNN a few days ago, and then there’s a lot of hype in terms of having colorectal cancer in young patients, but they’re really not genetic abnormalities, but it really points to these non-genetic abnormalities we have to pay attention to as well. So what can we do? Dr. Budde is absolutely correct in the sense of we should be able to enroll patients on lung cancer trials. Many of you have those here in Southern California and across the nation and across the world. Again, this is a laundry list. I don’t expect everyone to read this, and there’s no quiz at the end, so don’t worry.
But at the same time, we know that we need to go forward and we need to be able to still cure non-small cell lung cancer in the metastatic setting. And in a TKI setting, you have lots of resistance where you don’t really see cure, but control. But then at the end of the day, how do you define cure? If a patient has no evidence of disease after 7 years or 10 years of getting Osimertinib, is that a cure or is that a control? And I think we need to redefine some of the definitions we have. So going beyond EGFR is a receptor tyrosine kinase. We know KRAS, the code has been broken, especially for G12C. We know that there are a lot of KRAS abnormalities that can occur and we clearly know G12C is important, but so is G12D and G12V, Q13 is important, Q61 is important, Q146 is important for KRAS. These are all important in terms of your decision making for precision medicine and personalized medicine. And here’s just a summary of some of this data that occurs. Within the various tumors as well as within lung cancer itself. We know that there are a number of therapeutic approaches one can use, such as the neoantigen vaccine that has been used by the NCI. Direct KRAS inhibitors will talk about that in a minute, but we also know downstream signaling is important.
So phosphatase such as Shp2 (phosphatase 2), that’s a 68 kilodalton protein, that’s important as a downstream for KRAS, but we also know that you can have other downstream signaling molecules that you can target, such as Paxillin, which is a focal adhesion kinase downstream target. At the same time, ICIs work pretty well for KRAS unless you have other abnormalities such as MDM2 amplification or STK11 abnormalities or other abnormalities that we, or KEAP1 abnormalities as an example. So here are some of these lung cancer trials that are ongoing, and you can find them certainly in Southern California as well as throughout the country. . But at the same time, we know that these KRAS inhibitors work and they work well, but only up to a time.
And then I come back to that mechanisms of resistance with KRAS inhibition that we have to pay attention to as well. So here’s the first study that was presented. Phase 1 was done and then thereafter phase 2 was reflected in, Sotorasib. But you can appreciate the median progression-free survival is only 6.8 months. This is second line type of study and we have to be really be aware of this because even though this was breaking the code, but it’s not good enough for us and we have to continue to do go forward in this context. Similarly, at Adagrasib at very similar results, you can see that the median progression-free survival on the right is 6.5 months. And the overall survival is 12.6 months. Again, our patients deserve this drug, no question, along with Sotorasib and other drugs that are being developed. But in my mind having practiced for so long, not good enough, and we need to make it better for our KRAS patient. So here’s the dilemma we all have, many patients, if not all, may develop resistance. So how do you define these resistant mechanisms? You have to think about genetic resistant mechanisms and genetic resistant mechanisms in KRAS for non-small cell lung cancer. If you read the papers that have come out in Nature as well as namely Journal of Medicine, especially for Mark Awad and other colleagues over at the Farber. You see That in non-small cell lung cancer, you don’t really have these genetic abnormalities except for other KRAS mutations that can occur or MET amplification That can occur, but that only happens in about 10 to 20% of the time. So that leaves us to non-genetic mechanisms of resistance, and we need to pay a lot of attention to that and be able to overcome that. Again, on the right is a cartoon diagram that shows this primary resistance versus acquired resistance, but the genetic non durable response in a tolerance state and then acquiring resistance is quite important. I emphasize this continuously because people ask us is, what is the future for non-small cell lung cancer? It’s really understanding the mechanisms of resistance and overcoming it. De novo or Ipso facto after therapy itself. We also know that there are large number of lung cancer trials that are ongoing and there are PAN KRAS inhibitors that are G12C inhibitors. A number of inhibitors will come for G12D as well as G12V, but then we have to worry about the other codons as well, like I said, like codon 13 and 61. So all of these studies are ongoing and we’re very much looking forward to the various trials themselves.
So we did EGFR, we did KRAS, I think this is a whirlwind tour. We’re going across the country and across the world, and we’ve just really talked about a lot of discoveries that have been made, but ALK has been one of the greatest discoveries as well. ALK fusion such as EML4, ALK occurs on chromosome 2p that was initially described, in a Japanese patient by Dr. Noda and colleagues in their Nature paper, where they showed in a young Japanese male with a cignet ring cell phenotype that had an EML4 ALK, a fusion and responded ultimately to a TKI, and Crizotinib was the first TKI that was discovered. Crizotinib, as you remember, is, was used to be known as PFO2341066, and I remember that because 1066 is the battle of Hasting. So any history fans can really appreciate true chemistry that gets developed and how things get named as well. So when ALK rearrangements can be detected by fish, by NextGen sequencing, by meniscus chemistry, but you can see these ALK fusion partners. It’s not just EML4 on the right, but it’s KIF5B, TFG, and others. And do they respond to the therapeutics versus non therapeutics is a very big question as well. Here’s the timeline for alk inhibitors. Timeline for ALK inhibitors was incredibly fast. So as a timeline for met, which I don’t talk about, we initially discovered the MET Exon 14 in really 2001, but therapeutic fruitions really came over the past decade or so. That was a long-term discovery. Whereas ALK discovery was initially, like I said, was described by Nota and colleagues in 1994, and then EML4 ALK was rearranged, I’m sorry, the 1994 was anaplastic large cell, but nothing happened for non-small cell until 2007. And then certainly we were quite involved and I was one of the first ones to help write the protocol for Crizotinib, and we got that approved through the FDA after only a phase 1 clinical trial. Crizotinib was a great drug except it didn’t cross the blood-brain barrier as well as we should have. You see these millary pattern of brain metastases that can occur in out positive tumors. We also see that the potential for metastasis in a tumors is completely different as compared to other tumors that we see. So they can actually go onto the ANXA so you can have it metastasized to the uterus, to the ovaries that we’ve seen. It can metastasize to the stomach, it can metastasize to the peritoneum, and you can’t really reproduce that in the mouse model. It’s only the human model that you see that as well. And then certainly a lot of other drugs have come to fruition. We’ll talk about right now is to be able to say that you have Crizotinib then Ceritinib, Alectinib, Brigatinib, Lorlatinib, and at the same time, Lorlatinib has been really powerful in terms of its overall response rate as well as overall survival and PFS. And certainly that’s one of the drugs that one can use. And here’s one of the rationale for utilizing Lorlatinib in the first line setting, but it can be used in second line, third line setting as well. There are many mutations that occur. I tend to, when we have fellows as well as students in the room with us, with patients without positive tumors or EGFR. We always say you have to really know these mechanisms and the therapeutic responsiveness. And at the same time, you have to be able to have a cheat sheet with you in the clinic room to be able to say it’s an ALK fusion, but it’s not an EML4 ALK. And how should we choose our drugs? And these are some of the ways that we can do that by preclinical data selections as well. Again, mechanism of resistance, genetic versus non-genetic. Genetic. You can have gatekeeper mutations that are important, and it’s very important to do your liquid biopsies, your biopsies, do next gen (NGS) sequencing after disease progression for patients so that you can really select out these drugs. Again, this is a little bit more complex in terms of signal transduction, but the theme is there. The theme is that you can have genetic alterations and you have to be cognizant of that, and then you can give therapeutic re therapeutics based on that. The non-genetic is tougher because we don’t understand it at this point, but certainly if you have MET overexpression, you can think about other drugs that are being developed for MET as well.
So last thing I wanna talk about is immunotherapy. Again, not enough time to talk about everything, but we all talked about earlier today, PD-1 as well as anti PDL-1, quite important. And here’s the timeline for various approval. Lung cancer, it’s great. When I started my career, it was Carboplatinum, Paclitaxel, and Hospice (or palliative care). You didn’t know who was gonna respond, who, and you even had phenomenal colleagues who were able to do biopsies such as radiology or surgery or pulmonary. But they would tell the patients, oh, don’t go to the MI oncologist, just go to hospice if you have stage four disease. Been there, done that. And so fast forward 30 years now, and we have so many incredible approvals for various drugs for non-small cell lung cancer. That it represents the paradigm for precision medicine and clearly the overall survival and the PFS for chemotherapy IO versus IO alone is reflected here. But I wanna show you what has happened with all these clinical trials for immunotherapy itself. So as an example for Keynote-189, that was chemotherapy or immunotherapy, chemotherapy, and you can even see 5 year survival. Who would’ve thought in our career that we can say, talk about 5 year survival and cure for metastatic non-small cell lung cancer? I think small cell is still a holy grail for us. We need to put a lot of time and effort into it, but at least a large subset of non-small cell lung cancer can be targetable or they can get immunotherapy and you can have nice responses as well. And that’s a huge thing for our patients. But not only is Pembrolizumab approved, but Daratumumab, Ipilimumab in combination has been approved either by itself or in combination with chemotherapy. As you can see from these graphics themselves, Cemiplimab is the new kit on the block as well, and that has been approved for first line setting as well. And this is the EMPOWER-Lung 3 data set, which is reflecting this 12 month overall survival versus the PFS, and clearly you can see the separation of the curves themselves. Most recently you also had Daratumumab and Tremelimumab that got approved, and that also brings to a point that you can have negative predictor for immunotherapeutic responses to STK11 or KEAP1. Sometimes MDM2 amplification and there can be hyperprogression with your patients who get this immunotherapy. That’s very clear and it’s not like melanoma where one can say there’s pseudoprogression in non-small cell lung cancer. I really don’t see pseudoprogression. We really see hyperprogression, so you have to keep that in mind, but can that hyperprogression be overcome by combinations of anti CTLA-4 as well as anti PD-1 or anti PDL-1? We tend to believe so, but a lot of this can be retrospective data analysis and we need to do a lot of prospective analysis. Here’s a, again, a summary diagram that we adopted from the Reck article, but then added on, you can have monotherapy such as Pembrolizumab, Atezoluzumab, Cemiplimab, or combination therapies, and more and more are coming to fruition as you go into FDA approval. And then we updated this in November, 2022, previously with the Cemiplimab chemotherapy as well, Durvalumab and Tremelimumab and chemotherapy, and again, more and more is coming. And how do you make a decision? You really have to make that personalized decision. You not only have to take into account the gender, the performance status and others, but you have to take the molecular abnormalities into account as well. So here’s a, again, a simplistic first line treatment algorithm. Take it with a grain of salt because I may follow it and I may not follow it. And it really depends on your decision making in that clinic. It’s nice to have all these clinical trials, but we don’t really incorporate the geriatric populations into clinical trials, that’s important. We don’t incorporate the poor performance status patients into our decision making. We don’t incorporate somebody who has thrombocytopenia or let’s say nephrotic syndrome and how we should deal with that. How do we deal with perineal plastic syndrome? Those are all realities in our clinical decision making. So at least what one can think about is non-small cell lung cancer treatment algorithm. Are they PD-L1 less than 50% or PD-L1 over 50%. We can have large argument, is it the 22C3 versus the 28A versus the SP of 142 versus the SP263. These are all immunohistochemistry antibodies and which one is the right one to utilize? At least this gives you a little bit of a sense if you were to follow some guidelines that these are some of the things to be able to say immunotherapy by itself versus immunotherapy in combination versus in combination with anti CTLA-4. Again, the field is gonna get even more complex and that is to be able to look at the current and potential therapeutics in non-small cell lung cancer. And you can see all of these drugs that are being developed, all of these pathways that are being considered. And you have to think about it in an early stage two, do you combine that with radiation therapy? Do you combine that ipso facto surgery? Do you do pre therapy before surgery? So like neoadjuvant, which I didn’t talk about, and that’s here to stay as well. And so as you think about non-small cell lung cancer itself, It’s a very heterogeneous disease. Dr. Budde presented very nicely lymphomas and there are so many different types of lymphomas. Same thing with sarcomas, same thing with non-small cell lung cancer. And there are a number of actionable targets giving better PFS and OS, and the mechanisms of resistance are very important to understand and we need to be able to sentence all of our to sequence all of our patients themselves. I say all of this data in a very quick fashion. I’m actually on time itself, but I also feel like I’m a reporter. I’m reporting on the activities for City of Hope for all of my colleagues. I want to thank all of our colleagues. Many of my colleagues are here from City of Hope and obviously from other places as well. So nice to see everybody and we should take a group picture if I can suggest something. And at the same time, our laboratory is very important as well for the structure function, mechanisms of resistance. So I do want to thank the organizers for inviting me, and thanks to the board as well. And thank you all for coming as well, and I’m happy to take questions.
What is EGFR, KRAS, ALK and immunotherapy for non-small cell lung cancer (NSCLC)?
Non-small cell lung cancer (NSCLC) is a common type of lung cancer, and several molecular targets have been identified that can be exploited for therapeutic purposes. Among these targets, EGFR, KRAS, and ALK mutations are the most common, and recent clinical trials have explored the efficacy of targeted therapies against these mutations. Additionally, immunotherapy has emerged as a promising approach for treating NSCLC.
EGFR mutations are present in approximately 10-15% of NSCLC cases and can be targeted with EGFR tyrosine kinase inhibitors (TKIs) such as erlotinib, gefitinib, and osimertinib. These agents have demonstrated improved progression-free survival and overall survival in patients with EGFR-mutant NSCLC. However, resistance to EGFR TKIs can develop, and new strategies to overcome this resistance are under investigation.
KRAS mutations are present in approximately 20-25% of NSCLC cases, but effective targeted therapies for KRAS-mutant NSCLC have been elusive. Recently, efforts to develop KRAS inhibitors have shown promise, and early clinical trials of KRASG12C inhibitors have demonstrated clinical activity in a subset of patients with KRAS-mutant NSCLC.
ALK rearrangements are present in approximately 5% of NSCLC cases and can be targeted with ALK inhibitors such as crizotinib, ceritinib, and alectinib. These agents have shown efficacy in both treatment-naive and previously treated patients with ALK-positive NSCLC.
Immunotherapy has also emerged as a promising approach for treating NSCLC. Checkpoint inhibitors such as pembrolizumab, nivolumab, and atezolizumab have demonstrated improved overall survival in patients with advanced NSCLC, particularly those with high levels of PD-L1 expression.
In summary, targeted therapies against EGFR, KRAS, and ALK mutations have demonstrated efficacy in NSCLC, and efforts to develop new strategies for overcoming resistance to these therapies are ongoing. Additionally, immunotherapy has emerged as a promising approach for treating NSCLC, and further research is needed to identify predictive biomarkers and optimize treatment strategies and be aware of possible side effects.
Ravi Salgia, MD, PhD – About The Author, Credentials, and Affiliations
He then did a fellowship in hematology and oncology at the University of California, Los Angeles (UCLA). During this time, he became very interested in thoracic oncology. He then did a fellowship in hematology and oncology at the University of California, Los Angeles (UCLA). During this time, he became very interested in thoracic oncology.
Through his groundbreaking research and clinical work, Dr. Salgia has worked hard to move the field of thoracic oncology forward over the course of his career. He has written many papers that have been published in the New England Journal of Medicine, the Journal of Clinical Oncology, and Cancer Research, among others. He has also been asked to talk about his research at many national and international conferences.
Dr. Salgia’s clinical expertise is highly sought after, and he has been recognized as one of the top oncologists in the United States by Castle Connolly and U.S. News & World Report. He is also a member of many professional groups, such as the American Society of Clinical Oncology, the International Association for the Study of Lung Cancer, and the American Association for Cancer Research.
At the City of Hope, Dr. Salgia serves as the Chair of the Department of Medical Oncology & Therapeutics Research as well as the Associate Director for Clinical Sciences in the Comprehensive Cancer Center. In these roles, he is in charge of overseeing clinical trials, coming up with new treatments for cancer patients, and giving his colleagues expert advice.
Overall, Dr. Ravi Salgia is a highly accomplished and respected physician-scientist whose work has had a significant impact on the field of thoracic oncology. His hard work to improve cancer treatment and patient outcomes has won him the respect of his colleagues and the thanks of many patients and their families.