ASCO [2022] Genitourinary Cancer(s): MOASC Oncology Spotlight
Dr. Arash Rezazadeh’s MOASC 2022 Presentation in Genitourinary Cancers (ASCO genitourinary cancers symposium)
ARASENS Trial – In Patients with Metastatic Castration Sensitive Prostate Cancer(s) (Genitourinary Cancers)
ARASENS (retrospective study) was one dataset that may change the standard of care for some of the patients with prostate cancer(s). So I picked that for that reason. It’s Darolutamide versus placebo in combination with ADT docetaxel. So remember the. The standard of care in this trial was defined as ADT plus Docetaxel, and it was in patients with metastatic castrate sensitive. Prostate cancer(s) (castration resistant prostate cancers) and patients were randomized 600 each 650 each in each arm.
Â
And they continued until toxicity or unacceptable toxicity or progress. So endpoint’s first endpoint was overall survival, which in this trial was met. The second endpoint was time to castration resistant prostate cancers, which I think is a very important outcome. And I will show you the slide on how much difference it made to add Darolutamide to chemotherapy and ADT.
Â
Time to pain progression and SSE-free survival (Symptomatic skeletal event free survival), skeletal-related events, and basically initiation of subsequent anti-cancer therapy. You’re trying to push the chemotherapy out by basically giving it early in for more fit patients. The patients can tolerate this rather than being sick after a few lines of (targeted) therapy.
Â
That’s why it’s important to think about the subsequent (genitourinary) cancers. Time towards physical symptoms and opioid use and finally safety. Again, these are the patient characteristics, mainly white, and some other ethnicities are mixed here. As you see, the region in North America, Asia, and the rest of the world is important too.
Â
Have that information because subsequent (targeted) therapy can be different in the rest of the world and not necessarily the same in us and elsewhere. And then, you see the metastatic status at the time of diagnosis. If they had M0, they were not De Novo metastatic, and metastasis happened later, or they were metastatic at the time of diagnosis.
Â
And then alkaline phosphatase has been another category that we’re looked at. This is the overall survival primary endpoint. So the addition of Darolutamide to ADT plus Docetaxel significantly reduced the risk of death, but 32% versus placebo. And that was, of course, significant 75% of patients in placebo armed received subsequent life-prolonging systemic therapy.
Â
We still see that 25% of them couldn’t receive the subsequent (targeted) therapy, and it could. Possibly because of the drug access and, in some cases, overall survival benefits observed across most subgroups. And these are the hazard ratio for those stratified by patients with metastatic stage at initial diagnosis for M1. It was 0.7 for M0 0.6.
Â
Again, this is an initial diagnosis, so it means De Novo verses, these are secondary endpoints, and most of them were met they’re a couple that had a non-significant P value, including time worsening of disease related physical symptoms. I think this lets me see if I can point. Yeah, this is a very important point in this slide set. So if you see time to castration resistant prostate cancers (genitourinary cancers), there is a big difference between the 2 arms.
Â
And we know when castration resistant happens, that’s where the time the clocks start ticking means that you don’t have much to offer. So pushing it out is very important. And at the end and I will tell you why that is important. Some of these patients who were on placebo and got docetaxel, like 25% of them, continued to be okay after 57 months.
Why is This An Important Point?
So maybe early docetaxel gives you something to push out the basic development of the castration resistance. And again, I think it’s a very important point, and I tell you, why is that important? So, for new safety signals, there wasn’t much difference between the treatment arm of any grade 3, 5 serious adverse events.
Â
Fibrin neutropenia 7.8 versus 7.4. Seizures were similar, and I want to get your attention here because patients who were on Darolutamide stay on the drug for much longer. It’s not just by incidents. We look at the exposure. Adjusted incidents mean that for a long time, you stay on the drug. The chances of somebody having a seizure are probably higher.
Â
So if you look at the exposure adjusted incidents, it’s very similar to 0.2 versus 0.1 similar rates of death due to treatment emerge, and these are the conclusions. Darolutamide plus ADT plus Docetaxel significantly prolonged OS versus placebo plus ADT plus docetaxel in patients with metastatic cancer sensitive prostate cancer (castration resistant prostate cancer) median overall survival was not reached versus 48 months.
Â
Overall survival benefit in both Innovo versus recurrent metastatic disease at diagnosis was shown. So there is an overall survival benefit in both types of patients, and the addition of Darolutamide significantly improved (significant improvement) secondary endpoints. And fewer AE rates were comparable between arms with no new safety signal observed.
Â
So maybe you knew about this dataset, but the question is should Darolutamide plus ADT plus Docetaxel become a new standard of care for patients with metastatic castration sensitive prostate cancers (castration resistant prostate cancers or genitourinary cancers). We have another dataset with piece one, which uses Abiraterone Prednisone plus Docetaxel in a similar patient population with De Novo metastatic prostate cancer (castration resistant prostate cancer).
Â
And there was androgen treated naively. And it shows overall survival, but high volume versus low volume disease is an important thing to remember: everybody needs Docetaxel, really. And the benefit in piece one, at least for the time being, has been shown. High volume disease. Those are the patients that we knew use Docetaxel in them because they’re at high risk for progression.
Â
Why Will There Be Debate On The Next Trial?
So there’s a lot of debate is what’s gonna be the next trial. Next thing to do to show that we really need to give patients Docetaxel. We didn’t control it. For ADT plus novel hormonal therapy in this, remember the standard is to give Docetaxel in this trial; maybe the standard is to give ADT plus hormonal therapy.
Â
And then the addition of Docetaxel to hormonal therapy. Should be the experimental arm, and then see if that Docetaxel adds anything. So the necessity of docetaxel still, in my opinion, is questionable. And basically, we didn’t test it in this trial. We tested the standard of care at the time of initiation of the trial, which was ADT plus Docetaxel.
Â
But the question is can anybody do this trial? Can we really randomize patients for this trial? Is it even ethical to do this trial?
So all those questions are there, but for the time. We have these 2 datasets, piece 1 and ARASENS. We suggest that the triplet can be something beneficial to certain patients.
What is Your Conclusion About ADT?
So these are the real conclusions. In my opinion, there is no role for ADT alone. Unless patients are not doing well, have a lot of comorbid, and we cannot really add anything to it. If the life expectancy is less than 2 years, that’s where you get the castration resistant. You can simply give them ADT and keep them going.
Â
Doubles of ADT plus novel hormonal therapy are applicable to all, of course, if they can tolerate it, except those with metastasis, which probably need Docetaxel. no role of ADT plus Docetaxel. I think it’s a very important message. At least in these 2 trials, we could show that the addition of hormonal to ADT (Androgen Deprivation Therapy) plus Docetaxel does something.
What Was Learned From These Trials?
That’s what we learned from these trials. So if you wanna give Docetaxel, you might as well give it with novel hormonal therapy. Patients are living longer with the diagnosis of metastatic cancers sensitive prostate cancers (castration resistant prostate cancer or genitourinary cancers), given many options. It’s time to optimize (pression free) survival while maintaining the quality of life.
Are they really maintaining the quality of life they get?
And that’s where the problem starts with giving chemotherapy to patients. Are they really maintaining the quality of life they get? It’s only an extension of their life. So the last part, we have this international perspective, open labor randomized phase 3 trial at UCI. We’re using basically the backbone of ADT (Androgen Deprivation Therapy) plus novel hormonal therapy.
EV-301 Cohort H in Patients with (Metastatic) Urothelial Carcinoma (Kidney Cancer)
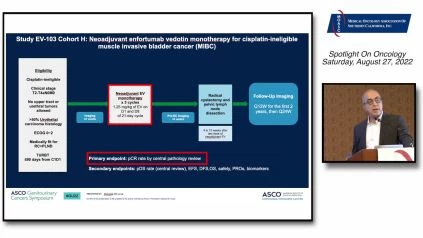
And we’re trying to see if the addition of PSMA-Lutetium-177 can be beneficial in this setting. So it is De Novo, in patients with metastatic disease, or patients who come with the previous local disease that has relapsed. Okay, for (metastatic) urothelial carcinoma progressing (kidney cancer). I chose to talk about EV-103 Cohort H, which is actually a neoadjuvant trial for patients who cannot receive cisplatin based chemotherapy in a neoadjuvant setting.
Â
So they received 3 cycles of EV (enfortumab vedotin monotherapy), prior to surgery. And these 3 cycles are actually every 3 weeks. So it’s not standard approved 4 weeks setting it’s day 1, day 8, and they get a week off and then keep going. So altogether, 3 cycles, 21 days, 9 weeks of therapy, and then get the radical cystectomy.
Â
And basically, the outcome was measured. Pathological complete (tumor) response by center pathology review, which is again very important to know. And you see the secondary endpoints as well. These are the patient population that you see listed here. Again, mainly white guys where we’re enrolled here. And the reason for cisplatin eligibility (or cisplatin ineligible) in kidney cancer.
Â
I think that’s an important point here. Why we put these patients on the trial and how we call them cisplatin eligible (or ineligible) and grade 2 hearing loss was about 40% of the patient. So this patient may be otherwise okay. Platinum only has hearing loss, about 40% of the. and creating clearance was about 50% of the time.
Â
Again, that’s between 60 and 30. And that criteria may be different from one practice to the other. Some people go with 50 or 45. Other drugs can produce PT0 with MVAC. The PT0 rate was about 38, 42, 31, and 46 with agents listed here. So roughly 30 to 40 percent of patients can have a pathological CR with different regimens, including the immunotherapy here.
Â
Dose based on clinical stage impact PCR?
And this is the first time using Enfortumab Vedotin as an agent in neoadjuvant. Dose based on clinical (settings) stage impact PCR? I think it does. And you can look at any trial. Also, the more advanced the patients are, the less pathologic CR you get. And these are listed here as you see in two different clinical trials with MVAC and Atezolizumab.
Â
So efficacy, pathological (tumor) response, a complete response for 36%, and downstaging was about 50%. So you can think about 86% maybe benefit. So when I say down, staging is not T2 anymore, so they have to be less than T2. So it means that if you have a T3 or T4, you cannot get T2 and send that down staging.
Â
So anything less than muscle invasive (bladder cancer) was listed. And it’s about to 86%. This is a small trial if you think about it. But again has a point that is tolerable for the patient’s preen neuropathy, about 27% with a short period of exposure to EV (enfortumab vedotin a neoadjuvant treatment), and rash maculopapular is a common thing, EV related is about 22%.
Â
Another important point is we did not make any patient ineligible for cystectomy, by exposing them to EV (enfortumab vedotin a neoadjuvant therapy), which wasn’t an issue because sometimes we give heavy chemotherapy to this patient, get in trouble, and cannot have cystectomy. All right, so ongoing phase 3 trials right now, evaluating new adjuvant therapy.
Â
VOLGA Trial From AstraZeneca – Durvalumab plus EV (Enfortumab Vedotin) and Tremelimumab (T)Â plus EV (Enfortumab Vedotin)
Are listed here, we are participating in the VOLGA trial, which is with AstraZeneca, and we are looking at the Durvalumab plus EV (Enfortumab Vedotin) and Tremelimumab (T)Â plus EV (Enfortumab Vedotin), so it’s a 3 arm trial with a cystectomy alone arm as well for patients who basically refuse chemotherapy. That’s important. What’s included in the inclusion criteria?
Â
The patient can refuse chemotherapy, or they cannot get cisplatin-based chemotherapy in a neoadjuvant setting. So there are a lot of trials going on in this setting, looking at the EV (enfortumab vedotin) and looking at the checkpoint inhibitors to see if we can replace cisplatin bases for patients who cannot tolerate or don’t do not want to have chemotherapy.
Â
So neoadjuvant EV (enfortumab vedotin) for UC comments: ADC development in earlier disease settings is rational. Can we go to non-metastatic, sorry, non-muscle evasive (bladder cancer), and all that? And PCR is impressive, but this is very important. The point will PCR translate to improve long-term outcomes and cure more patients. We know that with chemotherapy, but we really don’t know that for immunotherapy.
Â
We don’t know that for ADC. If they’re gonna translate, the PCR is gonna translate to long-term benefit for this patient. So PCR should be explicitly reported by baseline clinical stage means that you cannot put a bunch of patients with T2 and say, hey, this is performing better than MVAC because you have to look at the T3, T4, and patients who are higher risk of progression and see if you really downstage or get the T0 around those patient population.
Â
So eager to see the activity of neoadjuvant EV (enfortumab vedotin) plus immune checkpoint inhibitors. I talk about the trial we’re doing right now named VOLGA principle of PR precision medicine is again important, but you’re dealing with the earlier disease. We’re trying to see if we can really cure these patients. Maybe you want a more accurate one. Maybe you want to check for nectin, make, maybe you want to make sure that this drug has a target before.
What About KEYNOTE-564?
And I think it is very important to think about this disease to stay different than a metastatic disease as far as the side effects and efficacy of the drug that you’re given for (advanced) renal cell carcinoma. I have this adjuvant setting data KEYNOTE-564 adult with clear cell RCC (or advanced renal cell carcinoma, metastatic renal cell carcinoma) , intermediate-high risk, or M1, no evidence of disease. This patient has a mastectomy, after surgery, the first three months after the surgery, I define these groups here. The PT2 grade 4, a PT3 any grade will be intermediate high PT 4. And any, anybody with lymph node-positive would be high risk. And anybody who has evidence of metastasis is resected in the first place.
Â
Would be very high risk, and actually, we can look at it differently in patients, in a metastatic setting after metastasectomy, but remember, the resection of the metastasis should have happened in between the first year of diagnosis. So you could have it during the nephrectomy, right after nephrectomy (adjuvant therapy), or within one year of the development of, one year of nephrectomy, you could have the resected disease. So in this trial, Pembrolizumab was given for a period of 1 year versus placebo, and the endpoints were basically disease-free (progression free) survival. Primary endpoints have already been met on the first interim analysis. There was this number of events in both arms. As you see, 22 versus 30 median disease-free overall was not reaching either arm. It’s still early, and the key secondary endpoint was overall (progression free) survival, which we don’t have data for it yet. So maybe to you, it is old news, but I tell you, it’s gonna get more exciting. FDA approved this agent on November 17th, 2021, based on the first interim analysis and disease free survival rate in all 3 groups.
What Are The Hazard Issues?
You see the differences between the 3 groups. The hazard issue for the first group was 0.63 for all of them, M0.68 and M1 with no evidence of disease. That hazard ratio was 0.28 pretty good hazard ratio for somebody who had metastatic disease. And maybe those are the patients who benefit most from this adjuvant therapy in a clinical setting.
Â
You know that these patients most likely have some micrometastases somewhere, and maybe that’s why they benefited more compared to other groups in comparison. Overall survival update for additional 6 months after the initial interim results at 24 months. Again, that there were 23 in the Pembro arm at 43 in the placebo arm.
Â
Still not significant by definition because although the PE is low, the P was, had to be met, act much lower than this because they looked once in interim analysis again. Overall survival has not been shown yet. The adjuvant Pembro right now is only based on disease-free survival, and the data needs to be matured actually, their plan is to look at it for a longer period of time.
Â
So there was no safety update. After additional 6 months, there was no increased rate of steroid use because this patient pretty much was done, and they were going on other treatments if they had relapsed. So in conclusion, adjuvant Pembroke continued to demonstrate a DFS benefit versus placebo in participants with carcinoma with intermediate high or high risk or recurrence or M1 no evidence of disease after mastectomy after surgery with no new safety signal. This opt-in analysis of this study further evidence supporting adjuvant Pembro as a new standard of care for patients with renal ulcer carcinoma (advanced renal cell carcinoma) with (high) risk features of recurrence. Follow-up is ongoing for this trial.
CHECKMATE -914 Trial
So again, this is what we have right now, 1 trial disease free benefits in basically all subgroups and a different degree based on the (high) risk level. So this is the interesting part. We have that dataset FDA approval, but as you see CHECKMATE-914 trial had a press release on 7/29/22. And the combination of Ipilimumab and Nivolumab did not meet the DFS criteria.
Why Is This A Negative Trial?
So it’s a negative trial. If you give a combination of EVO, you don’t see the benefit, the R and B of the same trial in the same patient population. After a nephrectomy, high risk has Nivolumab versus plus placebo, which is ongoing, and the study of Atezo in the same setting will be actually presented at ESMO.
Â
So stay tuned for that to see those results they are under further investigation. And I wonder what’s gonna happen. Suppose that trial turns out to be negative. So you have 2 negative trials and 1 positive, and then how are you gonna think about giving these patients? Are there really different agents that we’re giving and or different populations?
Â
Is it trial inclusion or exclusion? What is it gonna be?
So stay tuned for more data. And as I said, CHECKMATE-914 is only a press release. It’s not really. We haven’t seen the data yet for that right now at UCI. We’re doing a trial in an adjuvant setting with Belzutifan, which is at AHF alpha inhibitor plus Pembro versus placebo plus Pembro.
Â
So everybody gets Pembro 1 group. The HIF alpha inhibitor with clear cell carcinoma, post nephrectomy (adjuvant therapy). So maybe additional therapy on top of Pembro gonna add more. We’ll see what this trial is gonna show us with that. I conclude my presentation, and thank you very much.
Dr. Arash Rezazadeh’s ASCO (genitourinary cancers symposium) 2022 Prostate Cancer Overview: MOASC Spotlight – https://oncologytube.com/v/41285
Â
Arash Rezazadeh, MD – About The Author, Credentials, and Affiliations
Dr. Arash Rezazadeh is an Associate Clinical Professor in clinical oncology at UCI Health and an medical oncologist who focuses their practice on the treatment of urologic malignancies.