ASH Meeting 2022 – Hematopoietic Stem Cell Transplantation with Tacrolimus Updates
By: Stefan O. Ciurea, MD – Director, Hematopoietic Stem Cell Transplantation and Cellular Therapy Program University of California Irvine
I was asked to talk about ab ASH updates and I selected 13 abstracts. I’m gonna go through them very fast if we’re already late. I have about 50 slides, first abstract I wanna talk about is this late breaking abstract, which is in fact first results from a randomized phase three trial done by BMT CTN. comparing two methods of GVHD prophylaxis with post transplantation, cyclophosphamide, Tacrolimus, MMF versus tacrolimus, methotrexate, what do I call conventional GVHD prophylaxis.
And this is again, a big study for us. There are not too many randomized studies in transplantation and this they randomized. 288 patients one to one. Actually 214 patients received post transplant cyclone Tacrolimus, m F, and 217 Tacrolimus methotrexate. So 400 30 patients.
Tacrolimus had at least 15% higher GRFS endpoint at one year.
Randomized one to one Primary endpoint was GVHD free relapse free survival. This is an GRFS. It’s a, it’s an a transplant endpoint. , which means that we want patients to survive without disease and without significant acute disease or chronic. GVHD primary hypothesis was the Tacrolimus F at least had at least 15% higher GRFS endpoint at one year, comparing with Tacrolimus methotrexate.
And briefly about this the the arm the investigation arm with post-transplant, cyclophosphamide, Tacrolimus and MMF was associated with better gfs, but this was not because necessary because improved in survival, but rather in decreasing significant decrease in day 100, grade three, four acute.
So disease from 14.7% to 6.3. There was no difference in relapse. Again, overall survival was similar. , there is a problem with this, unfortunately as probably many of we use Tacrolimus methotrexate plus ATG for unrelated donor transplants. This decreases incidence of GRA source disease in general.
I had a little problem with this because I feel that the control was not that greatly selected.
So I had a little problem with this because I feel that the control was not that greatly selected. I. In the sense that they did not add antiglobulin to the control. So these are the, this is the GVHD three relapse. We survive for these two groups. And again, post si arm did better.
Next is abstract number 115 impact of presence and amount of clonal plasma cells in the autograph for patients undergoing high risk myeloma. Patient undergoing auto autologous stem cell transplant. And this is data from MD Anderson Cancer Center. They looked at with using flow cytometry.
They looked at. Collected graph and again, this is for high risk multi myeloma patients by fish including one Q abnormalities. And they did eight collar NextGeneration flow cytometry of both of the graph and of the in the bone marrow. And they looked, they evaluated 416 patients. 75 or 18% had positive clonal plasma cells in the graph.
82% had negative plasma cells in the graph and ba Bottom line is that all outcomes were worse for patients who had significant plasma cells in the. graph. I’m, I feel like I, this needs to be a little farther away. Median progression-free survival overall survival and progression-free survival was better.
CR rates both for, they looked at both for patients who were in CR or VGPR versus less than VGPR. They found that outcomes across the board. So CR. Survival rates, relapse rates were higher for patients who had clonal plasma cells in the graph. And in multivariate variable analysis, the degree of clonal plus plasma cells, positivity in the autograph was independently predictive of worse progression phase survival.
These are the survival curve for different groups. Again, CR VGPR versus less than VGPR. And for all category, all this categories, survival was better comparing with the for those who had a clean graph versus those who had clonal plasma cells in the graph. Next abstract I want to talk about is, 2,101 allogeneic blood or marrow transplantation with high dose post transplantation cyclophosphamide for patients with a lll in older individuals above age 55 in remission with reduced intensity conditioning.
And this is data. These are data from , Hopkins. They looked at their older patients treated between January, 2008 to January, 2021 and compared above age 50 55 and look at primarily outcomes of patients in remission. They identify 77 patients. All of them receive post-transplant cyclophosphamide.
Most of them receive a hypo identical donor. Five year for the entire group, five year relapse and overall survival were 46% and 49% cumulative. Insulin of relapse was 27%, and non last mortality was 28%. Patients who received the myelo ablative conditioning, did significantly worse, had worse relapse-free survival as well as patients who received the peripheral blood graph as compared with bone marrow.
That’s why we also argue that patients with b with ALL in general should receive a bone milligram re, a bone marrow rather than peripheral blood stem. And they they describe particularly good outcomes at five years. Five years for patients in CR one with B-cell, ALL had a relapse survival of 61% and overall survival of 64%.
These are really good outcomes. For these patients and we are on the same page. We use we use actually a reduced intensity condition regimen for older patients here above age 55, I am, I’m even inclined to to use a lower threshold in general treatment related portal for patients with ll receiving a transplant goes significantly higher above age 40.
So above age 40 one could consider, especially for patients in first complete remission with negative. also 23 patients, pH positive ll received TKI maintenance second or third generation after transplant. And their five year relapse rate was only 5%. The only problem is that not all patients can tolerate TKI maintenance.
And in fact, there is another abstract that I’m gonna get to later on which shows that just that. But this small little figure here shows progression-free survival and overall survival shows overall five year overall survival for patients with B Cell ll in first complete admission by age 55.
Which again seems quite good. This is very important because it’s, it tells us a couple of things. Number one, older patients should, including for older patient , should not receive a myelo ablating condition regimen. Some may be tempted to do that to prevent disease come back. Seems like these patients, especially those in first completion with negative, but they do not need that.
Patients should receive a bone marrow graph.
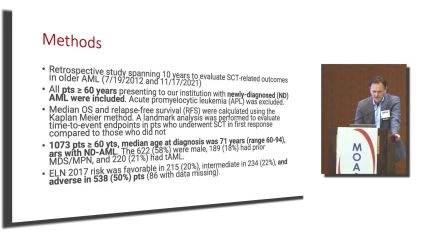
Patients should receive a bone marrow graph. There’s some important findings. Next abstract is 2,125 Allergenic stem cell transplantation in older patients with aml analysis over a 10 year period from MD Andone Cancer Center. This is in fact an analysis I started to do probably eight years ago with MD Anderson would never see the light because we.
We had our leukemia, we had two departments. We had a transplant department, and the leukemia department was never convinced that doing a transplant in older individuals is is a good idea. It and I studied this with Jorge Cortes, who was there long time ago.
And finally this came out, this analysis came out in Ansar format. And I’m gonna talk to you briefly about this. Patient. With newly diagnosed a l above age 60, we’re including the analysis. More than a thousand patients were analyzed here. Median age was 71 years range, six to 94, 94 years old.
Getting an oral transplant is quite something. And in remarkable, most patients had adverse e l n risk 50% of them. 84. So regarding initial treatment, 84% had low intensity regimens. 16 had intensive regimens. And more recently venetoclax was added in 34% of the patients and CRI rates were different, was 60% for the entire cohort, but was 74% for for intense.
48 for low intensity regimens and low intensity plus Venetoclax therapies, 72%. So this is quite remarkable. And shows that low intensity condition, we talked about oral asthma aza, for example, plus Venetoclax could potentially reach same CR rates with or without current recovery as intense condition regimen.
Watch and Share the Video Interview Here: https://oncologytube.com/v/41769
As most of these patients cannot tolerate intense condition rates, so it’s, I think it’s an important step. Referral for transplant, as I mentioned, was initially lower and has progressively increased over time from 31% between 2012, 2013 to 52% in 2020s. And as one would expect doing a transplant for patients who achieve CR or cr.
Upfront in order individuals was associated with significantly better survival of patients. So this they did a landmark analysis analyzing patients who went to transplant first remission and who did not. And and although patients who went to transplant had were younger of course, and had better performance from a disease point of view, groups were similar.
Survival was again better for those who underwent transplant in blue versus those who did not. Next abstract is 2001 17, consolidation with allogeneic stem cell transplant for patients receiving CAR T-cell therapy for a acute lymphoblasts leukemia. b-cell, ALL. This is data from city of.
This is this is not a big number of patients, but is there is they found a significant association much was previously reported between, for patient, they found better survival for patients who achieved CR CRI or disease control after CAR T who end up getting an allogeneic transplant versus who did.
and about half of these patients. Let’s see, how many patients were. Proceeding to transplant was at the physician discretion. About 50% of the patients here were taken to transplant in total. 58 patients were analyzed were underwent Luca, phase 46 patients received, in fact a car T and.
Among responders 12 month relapse, VIR was 81% for patients, had an allo transplant vir 16%, primarily because the fact that obviously most patients receiving CAR T alone relapsed in multivariable analysis. Only consideration with allo transplant was independently associated superior relapse phase.
And the hundred day no less mortality for the patients who went to transplant was only 5%. So the transplant was pretty well tolerated. And interestingly, there’s a good proportion of pa about uh, 60% of patients one, one car t in this analysis. Failed a first transplant. So these patients failed.
One transplant got CAR T and half of them end up getting an a second all and they. , they seem to do remarkably well in fact, because treatment related mortality can be significant with so much treatment. And two transplants. And these are the survival curve for curves. For patients who underwent allo transplant as consolidation therapy, postcard, T versus who did not.
Next abstract is number 360 2 is an oral abstract also from City of Hope about it clinical outcomes from a phase two clinical trial postal lu cell, which is an off-the-shelf multiverse specific T-cell therapy to prevent clinically significant viral infectious post trans. And I didn’t put it further up because there are some concerns with this.
The data is not that clear. So they they treated, I believe, 26 patients only with high risk to reactivate viruses such as hap identical umbi cords mismatch, unrelated donor mat, unrelated donor donors with low lymphocyte count before trans. At two weeks to maybe five weeks after allo transplant, they started to infuse these CTLs, which were generated against adenovirus, BK virus, CMV EBV, HHV-6, and JC.
and the goal was to try to prevent viral reactivation of the transplant and prevent clinically significant infections. And this is a little bit vague but they patients started to receive their first, again, as mentioned here, first c CT L infusion during this period of time.
And they continued every two weeks with another infusion threat to prevent reactivation.
Interestingly enough that eight patients or 31% had serious adverse event events and and there were some significant develop some significant some patients had significant development of acute grammar. Source is grade two to four at 31%, which is a little too high.
they detected the cells in vivo up to 12 weeks after the infusion. And they, while the viral reactivation was high similar to almost for, to patients that, that do not receive the cells, they claim that clinically significant infections were low. And I’m not sure exactly again, what that. Next abstract is number 3,442 haplo Donor Transplant for with post-transplant Cyclophosphamide for patients with MDS mpn.
And this is a retrospective study. There are no prospective studies like with this particular, for this particular group of patient with this particular. So I think this is a welcome. Abstract because there’s really no data on these diseases with HEOR transplants. And these are, again, a retrospective SIS of 14 centers who put to put together 114 patients with MDS, MPM cmml, atypical cml treated between 2010 and 2022.
They also had some NGS data on 85 of these patient. Here 51% has cmml 41 MDS mpn and the small number had atypical cml MDS, P n with ring Clasts endocytosis. Median h for this group was 62 million. Follow off for the entire cohort was 2.4 years range, between 14 days to 10 years. They found that outcomes were similar between all these, so they didn’t stratify this group when they analyzed because they, there was no significant difference for transplant between any of these groups.
And probability of three year overall survival was 56%, which is quite good. The last year survivors 40% treatment, 80 mortality, 27% relapse rate, 25. Interestingly, in multi analysis age at transplant, higher older age was associated with higher treatment, anti mortality as expected, and in large spleen was associated with higher relapse rate, and these patients had inferior survival.
Re reduced intestinal ablating condition was as while associated with higher relapse rate, had lower no less mortality with similar overall survival compared to more intes conditioning. And this is, these are the overall survival, relapse-free survival curves, relapse rate, and non relapse mortality.
Next abstract is again from City of Hope number 3371, frequent early geriatric complications after transplanting older individuals. And they looked at this outcome, this disability free survival for these individuals. They analyzed a large number of patients. All patients had greater than 60 years between 2013 and 2019.
And they tried to stratify patients that develop. weakness and mobility assistance early after transplanting five categories from independent assist assistive equip with necessitating assistive equipment necessitating person to assist both equipment and person and completely dependent and probably bed bound.
Also patients had a proportion of patients, so they did the disability included development of delirium. False ICU admission and mobility in addition to mobility assistance endpoint was this disability free survival. It’s unclear to me if included relapse or not is unclear from the abstract, but they look and see how many patients are basically.
Cured without having significant disability because I acquiring significant disability early after transplant is associated with the higher treatment rate, mortality and poor survival. 28% of 0.3%, develop assistance by day 21, very early after transplant and cumulative incidence of other disability events at day 30 and 100 were for false.
4.9% delirium, 24.3%, quite high ICU admission, 15%.
Day 30 and day 100 disability events were strongly linked again to treatment related mortality and survival. And they did a landmark analysis and showed the patients who did not have. Day 30 disability events had significantly better survival, nor less mortality, significant survival.
So couple of things here. Number one, this is a significant drop in the first month after transplant. As you can see here, this is probably mostly. Disability plus streamline. This is disability free survival, upper minor disability free survival estimates. Yeah. So there is a good proportion of older patients that develop this disability and or mortality or end up having high mortality because of this and this tip dropping curve is a concern and patients who did not develop significant disability had really low treatment related mortality compared to the other ones.
So what we are, what we need to do couple of things. Number one, we’re trying, at least our institution are trying to decrease intensity of Mel and Melan Flu. Melan 140 s perimeter squares has been the standard reduced intensity condition, but in fact can be significantly toxic. In the number of patients I had patients who developed augmentation with this combo.
And they unfortunately do not recover. So what we did, we decreased the intensity of conditioning we’re trying to do to Mel for a hundred milligrams perimeter square, which which in fact we showed in a paper a couple of years ago that is a social significantly better survival in older individuals.
So one could potentially. Adjust condition intensity and not only to decrease this step to decrease early treatment related mortality and disability, which leads to high treatment related mortality in older individuals. Next abstract is 2058, allogeneic blood marrow transplantation using haploidentical grandchildren as donors for patients receiving haplo identical transplants with posite based GVHD prophylaxis.
Hopkins. abstract and they identify 802nd consequ consecutive adults receiving their first hap transplant between 2016 and 2021. 460. Received graphs from children, which is the prefer now source of stem cells for these older individuals. In general, we want to do their transplant with their children and 29 grandchildren.
And short, long story. Because patients who received a transplant with grandchildren were older. There was an apparent high treatment anti mortality, but when they did the propensity score matching between those who for and looked at the same kind of group of individuals, the results were not different at all.
And this is kapla meyer me survival estimates for. Patients with who received transplant, the grandchild versus with a child. Next abstract is about second allogeneic transplant disease, ebmt data retrospective or 1,550 patients. And what they’ve seen they looked they I’m gonna go briefly over the next few.
What the, this group reported that there has been a, an increasing number of second transplant, Andre, increased survival of these individuals over time. Interestingly enough okay. My time sounds like it is. We’re trying to keep on time maybe. Alright. I think that’s, but for the speakers, when you hear that sound, that means your time. Okay, thank you. Like share and subscribe here on Oncology Tube. Begin notifications when similar videos are available.
About The Author:
Hematologist Dr. Stefan O. Ciurea oversees the Chao Family Comprehensive Cancer Center’s Hematopoietic Stem Cell Transplantation and Cellular Therapy Program.
At the Grigore T. Popa University of Medicine and Pharmaceuticals in Iasi, Romania, Ciurea received his medical degree. In Harrisburg, Pennsylvania, at UPMC Pinnacle Harrisburg, he finished his internal medicine residency. After completing a fellowship in hematology-oncology at the University of Illinois at Chicago College of Medicine, he went on to the University of Texas MD Anderson Cancer Center in Houston for a fellowship in stem cell treatment and cellular therapy.
Ciurea spent more than ten years on the faculty of the Department of Stem Cell Transplantation and Cellular Therapy at the MD Anderson Cancer Center before moving to the Chao Family Comprehensive Cancer Center to oversee its program in hematopoietic stem cell transplantation and cellular therapy.
Ciurea has written more than 10 book chapters in addition to more than 150 peer-reviewed articles. In addition, he has held the position of primary investigator on numerous clinical trials, including trials that the investigator created. More than 50 gatherings and conferences all over the world have invited him to speak, often as the keynote speaker.
At the UCI Health Chao Family Comprehensive Cancer Center in Orange, he sees patients.
Professional Positions
Professor — Division of Hematology/Oncology, Department of Medicine, UCI School of Medicine
Director — UCI Health Hematopoietic Stem Cell Transplant and Cellular Therapy Program